While most pregnancies proceed without complications, as many as 1 in 5 women will experience a potentially life-threatening complication that requires the skilled intervention of a doctor or midwife. Among such complications is fetal malpresentation.
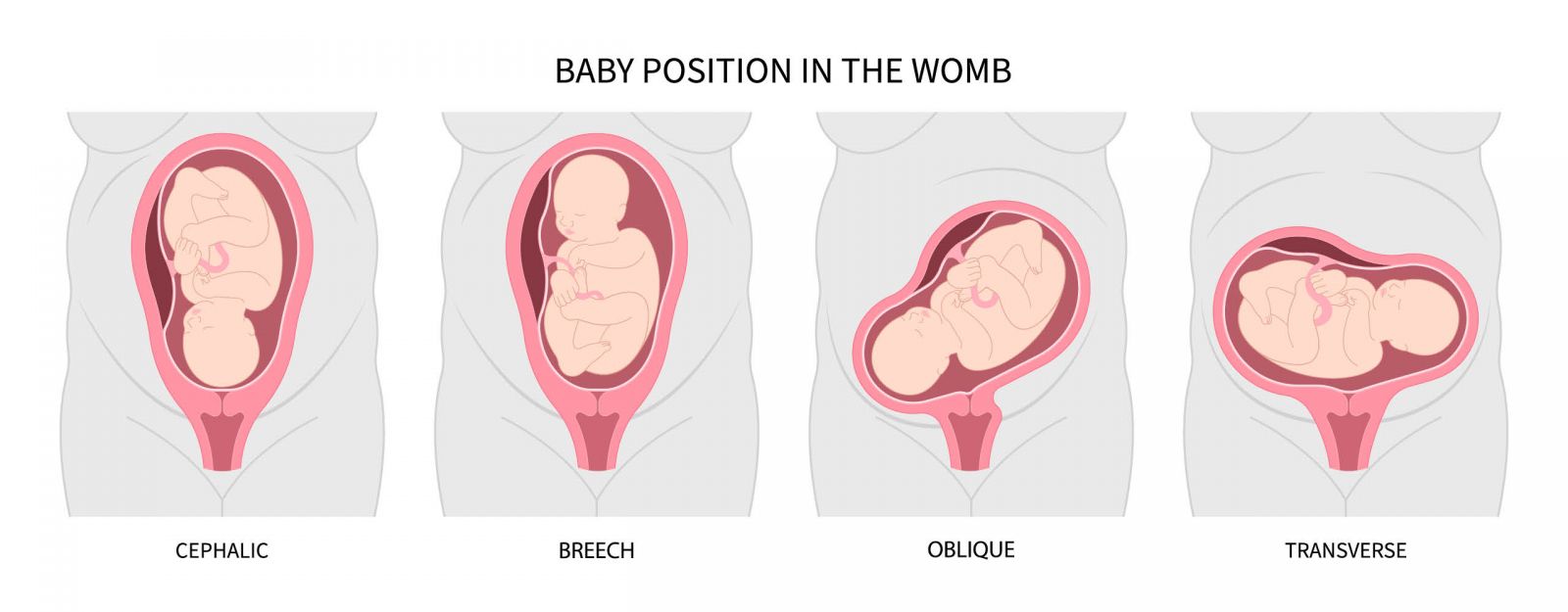
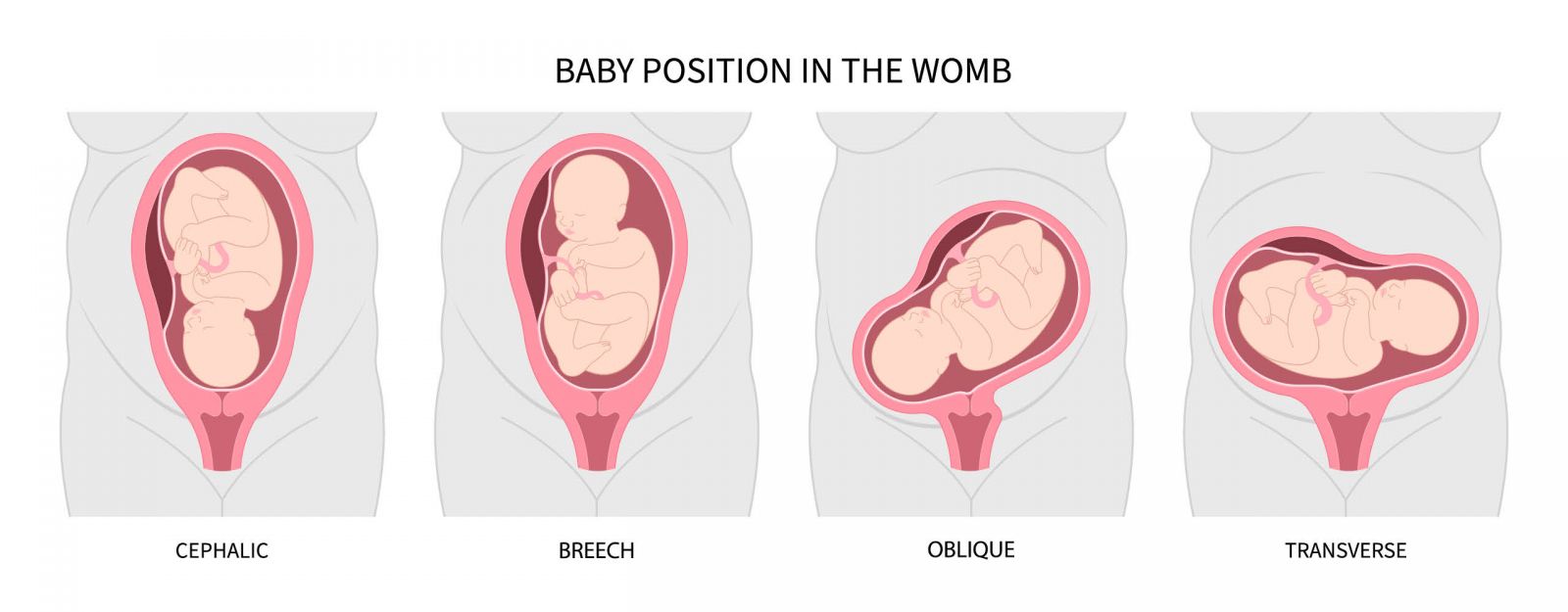
The cephalic position is the ideal and most common position from which to birth your baby, with its head down, facing your back, and its chin tucked into its chest. Most babies find their way to this happy spot between weeks 32 and 36 of pregnancy.
But sometimes babies don’t get into the right position at delivery, and complications of fetal malpresentation arise that make labor and delivery challenging for mother and baby, or require a c-section. Here’s what to know.
What Is Fetal Malpresentation?
Fetal malpresentation is diagnosed when the fetus is positioned in a way that ensures the first part of your baby to emerge from your womb is not going to be its head. The word “presentation” in this context refers to what part of the fetus is closest to the exit route through the pelvic inlet.
What Are the Types of Fetal Malpresentation?
There are several types of fetal malpresentation. Some may correct during the course of your pregnancy and even spontaneously during labor to allow for vaginal delivery, but others may require your care provider to reposition the baby or perform a c-section. Your baby will move around in your womb during the course of your pregnancy, but as it gets larger, its ability to move becomes more limited.
Breech
The most common fetal malpresentation is breech, which occurs when the baby’s bottom or feet are presented first. The breech position is typically seen in 3-5% of term deliveries [*]. It is more common in preterm deliveries. In twin pregnancies, 60% may have one fetus in breech position at the time of delivery [*].
There are 3 different types of breech position:
-
Complete breech: baby is bottom first with its hips and knees flexed as if it were sitting cross-legged.
-
Frank breech: baby is bottom first with hips flexed but knees extended and feet near its head.
-
Footling breech: one foot or the other is pointed toward the birth canal.
A 2023 study looking at fetal biometry in 4,501 singleton births alongside incidence of breech presentation found that the infants that remained in breech position until term birth (37 weeks or more) differed significantly in their head and abdominal dimensions than those infants born in traditional cephalic presentation, and these differences were apparent from the 32nd week on.
Breech fetuses were lighter and shorter overall, with significantly smaller abdominal dimensions and shorter femurs. But they had significantly longer and narrower heads than their cephalic (head-first) counterparts. The study’s authors posit that the smaller size of breech babies may be a matter of natural selection, as large babies in breech position increase the risk of deadly complications. Breech births were slightly more common among female infants in this study [*].
Transverse
Baby is essentially perpendicular to the mother’s spine, laying sideways with its shoulder over the pelvic inlet and its head and feet left or right in the womb, respectively. Most babies in transverse lie are delivered by c-section.
Oblique
Baby is neither parallel nor perpendicular to the mother’s spine, but at an angle with the shoulder the closest to presenting. During labor, baby may shift to a traditional vertex presentation, or it could go the other way, to a transverse lie. Oblique and transverse lies occur very rarely, in .05% of deliveries at term [*].
Compound
When baby presents a foot or a hand along with its head, it’s called a compound presentation. Most often it is not a major cause for alarm and the baby can proceed with vaginal delivery. Occurs rarely, in .1%-.2% of deliveries at term [*].
Face / Brow
Baby’s neck is outstretched with its chin pointing up, presenting the face or brow. Face presentation is believed to occur in 1 in 500 or 1 in 1,000 deliveries at term. Brow presentation is even more rare, in 1 in 700 or 1 in 1,500 deliveries at term [*].
Cord
The umbilical cord is against the cervix. This is seen in only .018% of cases and the number is diminishing with better prenatal care [*].
What Is the Difference Between Malpresentation and Malposition?
While these terms are sometimes used interchangeably, they are different. Fetal malpresentation is defined by the fact that the baby’s part presenting to the pelvic inlet is not the vertex head. Fetal malposition occurs when the baby’s head is presented first but is not oriented facing down in the pelvis of the mother.
When baby’s head is facing up, toward your abdomen, it’s called occiput posterior, cephalic posterior position, or “sunny side up.” Occiput transverse has the baby’s head sideways to the exit. Occiput posterior and transverse types of fetal malposition are seen with more frequency in first-stage labor but only around 5-10% persist up to delivery [*][*].
There is also some research that argues that the use of epidural analgesia relaxes the pelvic floor muscles and weakens contractions in a manner that may prevent the mother’s contractions from getting the baby’s head to rotate anteriorly [*].
What Causes Fetal Malpresentation?
There isn’t always a concrete cause for fetal malpresentation, but these are some of the factors that enhance the risk of it:
-
An abnormally shaped uterus
-
Presence of large fibroids
-
Too much or too little amniotic fluid (oligohydramnios)
-
A low-lying placenta or placental abruption
-
Multiparity (twins or more)
Women at enhanced risk for malpresentation are:
How Common Is Fetal Malpresentation?
Fetal malpresentation is fairly rare. Overall, 90%-95% of babies present at term in the proper vertex manner [*]. The incidence of fetal malpresentation is higher among preterm infants because they’re delivered before they’ve had a chance to get into cephalic presentation in the final weeks before coming to term. The most common type of fetal malpresentation is breech.
Fetal malposition is more common. It occurs in 33-58% of women in the first stage of labor and persists in 12-22% of cases at delivery [*].
What Are the Signs of Malpresentation?
Fetal malpresentation is typically diagnosed through ultrasound scan during the course of pregnancy and monitored through to labor. Your care provider will palpate your belly, listen to fetal heart sounds, perform a vaginal exam, and possibly an ultrasound scan as well to understand exactly where your baby is positioned.
A pendulous abdomen with weak abdominal muscles may be one sign of a fetal malpresentation. During labor, a premature rupture of membranes coupled with a delay in the descent of the presenting part of the baby may also be a sign [*]. If the baby’s presenting part is too large for the pelvis, an arrest of labor may occur [*].
What Are the Risks of Fetal Malpresentation?
The risks to mother and baby from fetal malpresentation and malposition are more significant in some positions than in others, but any fetal malpresentation or malposition requires the care of a specialist. Here are some of the risks:
Cord Presentation or Prolapse
By far, the most serious risk. Without the head to block the exit from the womb, the umbilical cord may exit the womb first, cutting off blood supply to the baby or injuring the baby by wrapping around its neck or arms. The compression on the cord by the descending fetus leads to fetal hypoxia and bradycardia, which can cause fetal death or permanent disability (including cerebral palsy).
It’s a rare obstetric emergency that results in fetal mortality in less than 10% of cases [*]. That number used to be 32-47%, before c-sections and advanced neonatal resuscitation techniques. Still, cord prolapse in a home birth setting carries with it a mortality rate that is 20 times higher than that of cord prolapse in a hospital birth [*].
One study found the incidence of cord prolapse to be 5-10% in transverse lie, 3% in complete breech and 10% in compound presentation [*].
Prolonged Vaginal Labor
If the baby is sunny side up, it may result in a longer, more difficult and more painful labor.
Arrest of Labor
Labor may be arrested when the presenting part is too big to move through the birth canal.
Slightly Bruised Face
If the baby presents with face or brow, it can still be delivered vaginally but may have some bruising to its face which should heal without further intervention.
Shoulder Dystocia
When the baby’s head has exited the birth canal but the shoulder is stuck on the mother’s pelvic bone, it is considered a medical emergency due to the high risk of cord prolapse. If your doctor can manually move the baby to free its shoulders, vaginal delivery can proceed. Otherwise, a c-section will be needed.
Cesarean Section
If the baby is breech or transverse, especially if they are preterm, the most likely outcome is a c-section. That said, there are a number of manual rotation techniques doctors use to help baby get into the right position and avoid a c-section.
How Do You Manage Fetal Malpresentation?
There are a number of things you can do to encourage your baby to get into the cephalic presentation in the weeks before birth. These include:
Pelvic Rocking on Birth Ball
A 2019 Indonesian study of 114 pregnant women found that pelvic rocking exercises on a birth ball helped baby get into a cephalic presentation [*]. 87.8% of the women who did the weekly exercises and 78.9% of those in the control group who did not do the exercises had a normal cephalic presentation.
Fetal Stimulation
Your baby can hear music, talking, and sense temperature and light changes in the womb. A cold compress (or bag of frozen veggies) placed on your belly where baby’s head is may encourage it to seek a better position for delivery.
Webster Technique
The Webster Technique was developed in the 1970s. It is a chiropractic adjustment designed to relax pelvic structures and ligaments to help rectify fetal malposition. But the evidence here is strictly anecdotal, there are no quality studies to indicate its effectiveness.
Yoga
Yoga has a number of benefits in pregnancy. It stands to reason that maintaining your strength and flexibility while calming your nervous system can offset any number of pregnancy issues. Down dog, cat cow, puppy pose, and bridge pose may help baby shift in the womb to a more desirable position [*].
External Cephalic Version
During birth, doctors and midwives are trained in a number of techniques to move the baby where it’s feasible to do so. External cephalic version (ECV) is chief among these techniques. It involves applying pressure on the fetus through the abdomen. It is considered a reasonable option where the mother is in early labor, the presenting part is not engaged, amniotic fluid volume is normal and there are no contraindications to vaginal delivery.
ECV offsets the need for c-section in 66% of term pregnancies with breech presentation, and 58% across all fetal malpresentations [*][*]. ECV can be attempted when baby is in breech, transverse, or oblique presentation.
Keeping Your Family Safe
MiracleCord provides industry-leading cord blood and tissue banking. Global Health and Pharma awarded MiracleCord Best U.S. Cord Blood Bank for its combination of technology, service, and affordability.
Cord blood stem cells are used to treat many diseases including blood disorders like anemia and leukemia. There are more than 80 FDA-approved cord blood stem cell treatments and hundreds more in trials.
Cord blood stem cells are a better match than those from other sources and can often be used to treat siblings as well.
Learn more by downloading our Free Info Kit or call 888.743.2673 to speak to a knowledgeable representative.
The Bottom Line
Fetal malpresentation that persists up to delivery is rare, affecting roughly 5% of births.
Up to half of babies may take their time getting into a cephalic position, and may be coaxed along in the weeks before delivery with a birthing ball or other exercises approved by your doctor.
But if you know your baby is not in the right position and you go into labor earlier than expected, get to the hospital immediately.
DISCLAIMER: THE INFORMATION ON THIS WEBSITE IS NOT INTENDED TO BE USED AS MEDICAL ADVICE.The materials and information contained on the MiracleCord website is provided for educational and informational purposes only, and is not intended to, and does not constitute, medical or other health advice or diagnosis, and should not be used as such. You should not use this information to diagnose or treat a health problem or disease. If you are seeking personal medical advice, you should consult with a licensed physician. Always consult with a qualified health care provider regarding a medical condition.