Placenta previa is a potentially life-threatening condition affecting roughly 1 in 200 pregnancies. Here is what to know about placenta previa types, what may increase your risk of having it, and what doctors do to care for women affected by placenta previa.
What Is Placenta Previa?
Placenta previa is a condition diagnosed after 20 weeks, when the placenta remains attached low in the uterus, covering the cervix in full or in part — effectively blocking the baby’s exit from the womb via the birth canal. It is the leading cause of postpartum hemorrhage.
The word previa comes from the Latin words “pre” (or “prae”,) which means before, and “via,” which means way. It is sometimes spelled previa. In medical terminology, previa usually refers to something blocking the passage through the birth canal.
The placenta is a miraculous organ, the only organ in the body that serves two masters independently: it gives the mother the hormones she needs for her pregnancy while sustaining the infant with the oxygen and nutrients it needs to flourish. The placenta can attach almost anywhere in the womb and still nourish the infant.
Many women (as many as 15%) will have a low-lying placenta early in their pregnancy that covers the uterus to some extent, but as the fetus grows and the uterus expands, the placenta typically migrates upwards. When we say migrate, the placenta doesn’t actually move, but rather, grows toward the increased blood supply at the fundus while its lower portion regresses and atrophies.
The vast majority of low-lying placentas do not turn into placenta previa. Scientists estimate the condition persists in .3% to 2% of pregnancies [*]. It is becoming more frequently seen concurrent with the rise in c-sections, advanced maternal age, and assisted reproduction.
If the overlap over the internal os (the opening that leads to your cervix) is greater than 2.5cm early in the pregnancy, the condition is more likely to persist.
What Causes Placenta Previa?
Doctors don’t know exactly what causes placenta previa, but they do concur on the risk factors [*]. Chief among them is uterine scarring — from a previous c-section (69.1%), D&C (13.5%), or endometrial damage/uterine fibroids. This is because uterine scars offer an environment rich in oxygen and collagen, two things a fertilized egg looks for when implanting.
Other risk factors noted in a 2021 study include [*]:
- Having had 3 or more children (63.5%)
- Advanced maternal age (>35) (53.8%)
- Assisted reproduction (5.8%)
These factors also increase the risk:
- Maternal health issues such as diabetes or high blood pressure
- Smoking or cocaine use during pregnancy
- Prior placenta previa (2-3%)
- Multiparity (carrying more than one child)
- Being pregnant with a boy
Ethnicity also plays a role. Asian women are 86% more likely to have placenta previa than white women, and among Asian women, researchers see the lowest risk in Japanese and Vietnamese women and the highest risk in Filipino women [*][*].
What Are the Symptoms of Placenta Previa?
The most common symptom of placenta previa is painless vaginal bleeding that is bright red. Some women with placenta previa may experience some bleeding after sex or mild contractions. Other placental disorders, such as placenta accreta, vasa previa, and placental abruption, are also associated with vaginal bleeding in the second half of pregnancy.
But one of the things that make placenta previa so dangerous, especially in countries where ultrasound is not routinely performed as part of neonatal care, is that a third of women do not experience vaginal bleeding. Many have no symptoms whatsoever.
How Is Placenta Previa Diagnosed?
It is standard clinical practice to assess the location of the placenta during the second trimester ultrasound. Ultrasound has a sensitivity of 91% and a specificity of 97% to identify all forms of invasive placentation [*].
Placenta previa is initially diagnosed via transabdominal ultrasound, but transabdominal ultrasound (over the belly) may not be precise enough in some instances. Transvaginal ultrasound is often indicated to give your care provider a better idea of exactly where the placenta is in relation to the internal os, especially when the placenta is located posterior and low lying. Transvaginal ultrasound is believed to be safe even in the presence of active bleeding [*].
Women who have a low-lying posterior placenta are more likely to have placenta previa than those with an anterior low-lying placenta. Transvaginal ultrasound may change the initial diagnosis in 1 in 4 cases [*][*][*].
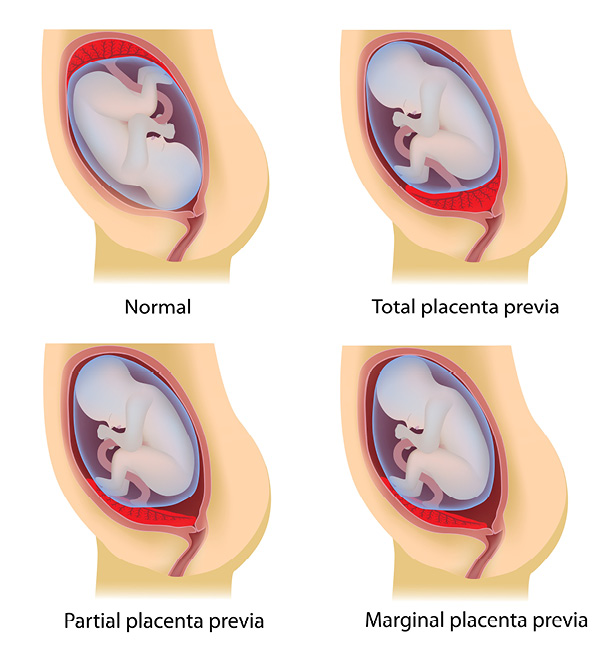
Types of Placenta Previa
Placenta previa types are distinguished by how much the placental edge overlaps the internal cervical orifice in late pregnancy.
- Complete placenta previa: The placental covers the internal os completely.
- Partial placenta previa: The placenta covers a portion of the internal os.
- Marginal placenta previa: The placenta is not covering the internal os but just outside it.
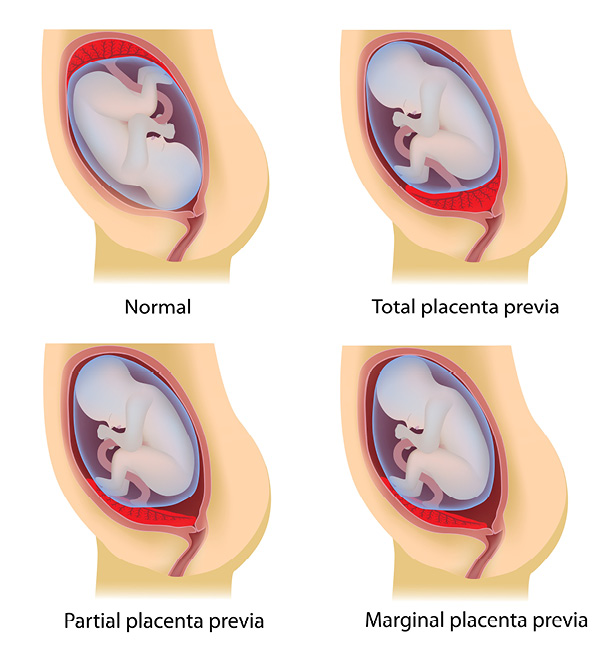
The terminology seems simple enough but can be confusing because these classifications aren’t always the standard used in research literature. One reason for this is that it can be hard to distinguish partial from marginal placenta previa in the absence of cervical dilation [*].
Some research simply distinguishes total placenta previa from partial, or placenta previa from low-lying placenta: Placenta previa may be used to describe when the placental edge overlaps or is within 2cm of the internal cervical orifice in late pregnancy. If the placental edge is located further away than 2cm but within 3.5 cm from the internal cervical orifice, the term “low-lying” may be used.
The simple way to look at it is, the risk of bleeding increases as the distance between the placental edge and internal os decreases [*].
Researchers have also studied the placenta previa types not only by how much the placenta covers the cervix but whether the location is anterior or posterior. Some studies indicate that women with full placenta previa and an anterior placenta location are at greater risk for preterm delivery related to antepartum hemorrhage [*]. But placenta previa is more likely to persist after 20 weeks when the location is posterior.
In considering how to manage these placenta previa types, your doctor will also consider whether you are asymptomatic, have active antepartum bleeding, or are stable after one or more episodes of antepartum bleeding, and how far along you are in your pregnancy.
How Is Placenta Previa Treated?
There is no treatment that can move the placenta from where it has implanted in the womb. If the placenta previa is marginal, or the placenta is diagnosed as low-lying, your doctor may recommend vaginal delivery to avoid future complications associated with c-section scarring.
In cases where the placenta blocks the cervix, digital vaginal exams and speculum exams are not performed and an elective c-section is planned for delivery.
Prior to delivery, vaginal or c-section, your care team may recommend a care plan to minimize bleeding and help you carry the baby as close to term as possible. This may include additional sonography (at 28-30 weeks and 36-37 weeks) to monitor the location of the placenta, umbilical cord, and any signs of fetal distress. Your care team may also advise you to avoid strenuous activity, heavy lifting, vaginal exams, or penetration. (See our self-care plan of placenta previa do’s and don’ts for more information.)
In more severe cases, you may be assigned bedrest at home or in the hospital and given medication to hasten the development of the baby’s lungs.
Possible Complications of Placenta Previa
Placenta previa, left undiagnosed, may result in the death of both mother and baby if vaginal delivery is attempted. The mother can hemorrhage, requiring blood transfusion, experience bladder injury, or even require hysterectomy. Other complications include:
Increased Risk of PAS Disorders
Placenta previa is widely believed to increase the risk of placenta accreta spectrum (PAS) disorders, severe maternal complications in which the placenta does not detach spontaneously after delivery and cannot be removed without causing massive hemorrhage or organ damage. Hysterectomy is often indicated.
The biggest risk factor for PAS is a prior c-section in combination with placenta previa [*]. While c-section rates have risen from 10% to more than 30% over the last 40 years, during that same time, there has been a 10-fold increase in the incidence of PAS, according to a 2020 study [*].
How deep the placenta has invaded in PAS affects maternal mortality, and it is not easily seen in sonography or MRI. It is both difficult to diagnose and to manage when discovered. While it is still rare, it is clearly on the rise; The incidence of PAS is expected to increase to 1 in 200 women undergoing c-section by 2025 [*]. Women who have a c-section scar, as well as a diagnosis of placenta previa, should speak to their care team about PAS.
Preterm Delivery
Preterm delivery is the most common complication associated with placenta previa. It is associated with a low-lying placenta, too, but to a lesser degree [*]. About 5% of all preterm births are due to placenta previa.
In future pregnancies, women with placenta previa who deliver preterm, especially before 34 weeks, are at increased risk for another spontaneous preterm birth regardless of where the next placenta implants [*].
Adverse Fetal Outcomes
For the baby, placenta previa may result in adverse outcomes associated with preterm birth, including a three-fold increase in neonatal morbidity [*], respiratory distress syndrome, and admission to a neonatal care unit. There is conflicting data on whether intrauterine growth restriction is associated with placenta previa [*].
Miscarriage is not usually associated with placenta previa because most miscarriages occur before the second trimester, when placenta previa can be diagnosed.
Can I Collect Cord Blood If I Have Placenta Previa?
Cord blood and tissue can be collected following a c-section delivery or a vaginal delivery, if the latter option is appropriate for you. Our StemCare® Collection Kit includes a sterile cord blood collection bag that is safe for use in the sterile field should a c-section be necessary.
In scenarios where there is unexpected bleeding during delivery or other complications, the first priority will always be to stabilize the mother and baby before collecting cord blood. If for any reason your care team cannot manage the cord blood collection, you will not be on the hook for any processing, testing or storage fees with MiracleCord. Only the $200 deposit is non-refundable, as it covers just covers the cost of the medical supplies in the StemCare® Collection Kit and shipping of the collection kit to you.
To learn more about MiracleCord and cord blood banking, download our Cord Blood Banking Guide.
Conclusion
Placenta previa is a serious condition that is on the rise in the U.S. in tandem with the increased incidence of c-section, assisted reproduction technology, and advanced maternal age. It is still relatively rare and, in the absence of PAS, not likely to be fatal when treated by c-section.
If you’re planning to have more children, experts say it’s best to deliver vaginally if the placenta previa type is marginal or just low-lying to avoid scars that could elevate the risk of PAS (or other complications) with a future pregnancy.
Any woman experiencing vaginal bleeding, spotting, contractions, or pain during her pregnancy, especially in the third trimester, should contact her care provider immediately or go to a hospital. Placenta previa with active bleeding is considered an emergency.
As always, defer to the advice of your care team.
DISCLAIMER: THE INFORMATION ON THIS WEBSITE IS NOT INTENDED TO BE USED AS MEDICAL ADVICE.The materials and information contained on the MiracleCord website is provided for educational and informational purposes only, and is not intended to, and does not constitute, medical or other health advice or diagnosis, and should not be used as such. You should not use this information to diagnose or treat a health problem or disease. If you are seeking personal medical advice, you should consult with a licensed physician. Always consult with a qualified health care provider regarding a medical condition.