For most pregnant women today, it’s hard to imagine going through pregnancy without ultrasound imaging to monitor the baby’s progress and detect abnormalities characteristic of potential disorders. These images are the first red flag when there are potentially life-threatening issues for mother or baby.
From a purely emotional standpoint, before the belly begins to show signs of pregnancy, those iconic, black-and-white images of the developing fetus rendered via ultrasound imaging make the pregnancy suddenly seem very real.
How does ultrasound work and what does it measure? Are there different types of ultrasounds? When should I have an ultrasound? What’s the latest ultrasound technology? To answer these questions, let’s start at the beginning.
What Is an Ultrasound?
The word ultrasound refers to a pressure wave with a frequency beyond (“ultra”) what is detectable by humans. In obstetric ultrasonography, a device called a transducer directs these ultrasonic sound waves at the mother’s womb, where they bounce off the tissues and structures there like an echo. The transducer picks up these reflected sound waves and changes them into images.
In pregnancy, the ultrasound monitors fetal development and screens for potential problems for the fetus and the mother.
The first clinical use of ultrasound occurred in Glasgow in 1956, using a prototype modeled on an instrument designed to detect industrial flaws in ships. The Diasonograph, as they called it, was developed by Scottish OBGYN Ian Donald and an engineer named Tom Brown. It was 8 feet high and took up about a third of the scanning room, prompting many to call it, uncharitably, the Dinosaurograph. Nevertheless, it had by far the best resolution at the time.
The paper Donald and Brown published in the Lancet in 1958 on this new technology was like a shot heard around the world: from Denver to Deutschland, Vienna to Japan, Copenhagen to Australia, the race was on to advance and perfect this compelling technology [*].
By the end of the 1950s, ultrasound was routinely used in Glasgow hospitals, but it didn't catch on in British and American hospitals until the 1970s.
In the early days of ultrasound, clinicians could only detect the baby’s head. Today, with developments in ultrasound expertise and technology, ultrasound can reveal dozens of parameters critical to fetal health and development — in 2D, 3D, and 4D (quasi-video) images.
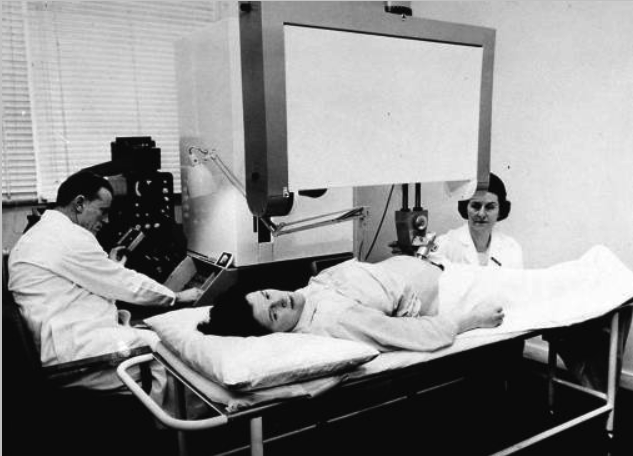
Ian Donald at work with the Mark 3 Diasonograph in 1960, jokingly referred to as the Dinosaurograph.
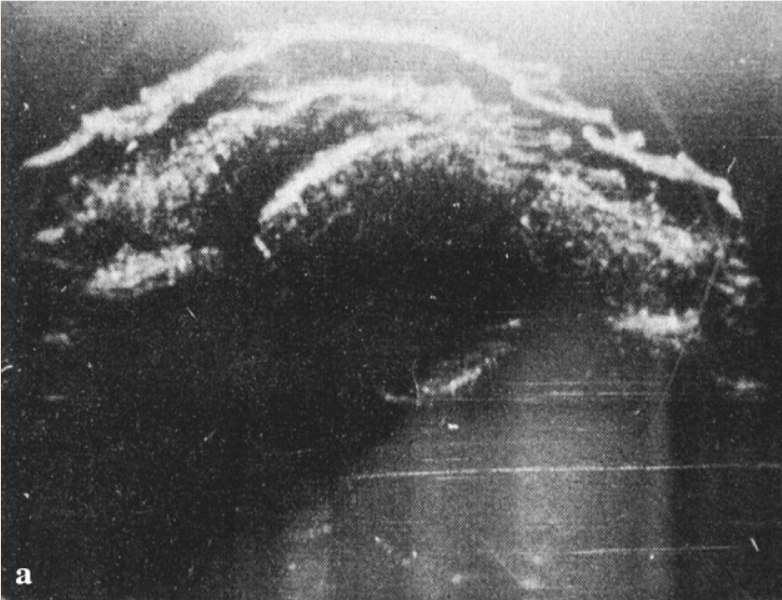
Image of the fetal head from Donald’s 1958 paper published in the Lancet.
Reasons for Pregnancy Ultrasounds
Ultrasound is the standard of care for screening for abnormalities and monitoring pregnancy because it is considered safe, noninvasive, painless, and yields immediate and extensive results.
Ultrasound helps doctors:
- Confirm you’re pregnant;
- Assess the viability of a pregnancy, meaning likely to carry to term;
- Check the fetus’s age and growth to determine the due date;
- Determine if there are multiple fetuses;
- Check fetal heartbeat;
- Screen for genetic abnormalities;
- Determine the baby’s sex;
- Capture detailed images and measurements of the baby’s limbs, organs, face, and spine;
- Diagnose ectopic pregnancy (when the fetus does not attach to the uterus) or miscarriage;
- Monitor the fetal support systems, like the umbilical cord, placenta, and amniotic fluid; and
- Determine the baby’s position before birth.
According to a recent Italian study, congenital malformations of different types and severity occur in 2-3% of fetuses in industrialized countries, leading to perinatal death in 25-30% of cases, and these numbers are increasing, largely due to the increasing number of pregnancies in women age 40 and older. That said, 80-90% of these fetal malformations occur in the absence of a specific risk factor for parents [*].
Early detection of abnormalities can optimize pregnancy management and save lives. According to Mayo Clinic, 10-20% of pregnancies end in miscarriage, though the number might be higher because many miscarriages occur before the mother even knows she’s pregnant [*].
It’s also worth noting that, even where the mother opts for an abortion, she may be required to have an ultrasound pursuant to state law, even if she doesn't want to see it. While many pregnancy care centers maintain that the ultrasound is medically necessary in abortion scenarios, the AMA Journal of Ethics argues it is not medically necessary and can add to the cost of the abortion procedure [*]. As state laws become ever more restrictive pursuant to the Dobbs v. Jackson decision, this requirement is likely to increase [*].
Is Ultrasound Safe for My Baby?
Ultrasound is considered safe — with certain caveats. Ultrasound is a form of energy and as such, may have effects on the tissues it traverses. Researchers know that high-power ultrasound waves are able to damage human tissue, but they don’t know exactly at what level this happens; testing this on human tissue is complicated for ethical reasons.
Researchers conclude that while ultrasound is a sound wave and can produce mechanical effects and temperature elevation in tissues it transverses, the risk to human fetuses is minimal when used only when medically indicated and with the lowest exposure time needed for accurate diagnosis [*].
Therefore, ultrasound scans should be used judiciously, where clinically justified, and in clinical settings. So while it may be tempting, for commemorative or bonding reasons, to do a keepsake scan at an elective ultrasound store in a non-clinical setting, you should avoid exposing your fetus unnecessarily to sonography — and exposing yourselves to the potentially inaccurate or even harmful information rendered by people with no medical training.
How Many Ultrasounds Are Done During Pregnancy?
Most women receive two ultrasound scans, in the first and second trimester, respectively, but the number and timing vary widely with the mother’s age, health, risk factors like history of miscarriage or birth defects, doctor’s preference, and symptoms like pain or bleeding.
In the first trimester, usually at 10-13 weeks, an ultrasound scan confirms the pregnancy and establishes the due date. In the second trimester (18-22 weeks), an ultrasound reveals the baby’s anatomy in great detail and its sex.
Women with high-risk pregnancies may be scanned earlier in the first trimester, 6-8 weeks in, when the fetus measures just around 2 cm.
In women with existing health complications like hypertension, diabetes, preeclampsia, or high BMI, additional ultrasounds may be indicated in the second or third trimester to ensure the fetus is maintaining its growth trajectory.
Additional ultrasounds may also be indicated to evaluate abnormalities detected in earlier scans, such as when the mother’s cervical length is shorter than expected or the placenta is considered too small, in a problematic location, or separated from the uterus (placental abruption).
Pregnancy Ultrasound Schedule
While ultrasounds can't detect all medical and genetic issues, they can illuminate physical characteristics associated with a wide array of potential disorders. Here’s what doctors look for with ultrasound at key points in your pregnancy:
First Trimester Ultrasound – Early (6 to 8 Weeks)
Check for a fetal heartbeat, forecast a due date, check for multiples, and check for ectopic pregnancy (a rare condition where the fetus grows in a fallopian tube or another area instead of the uterus).
Women with a history of miscarriage or pregnancy complications or otherwise at risk may have their first ultrasound 6-8 weeks into pregnancy. Early ultrasound scans are usually transvaginal to allow doctors to see the tiny fetus more clearly.
First Trimester Ultrasound – Normal (10 to 14 Weeks)
Measure the baby’s growth from crown to rump, confirm due date, and check for viability, genetic abnormalities, and certain heart defects.
For most women, this is the first ultrasound scan. At this scan, you should be offered a nuchal translucency test to evaluate your child’s risk of being born with chromosomal disorders such as Down Syndrome or Trisomy 18 (Edwards syndrome). The ultrasound portion of this test evaluates the thickness at the back of the fetus’s neck, with increased thickness suggesting a higher risk. The mother’s blood is also tested for specific hormones and proteins.
Your doctor will also examine the placenta, uterus, ovaries, and cervix, and look for any abnormal growth in the fetus. The baby’s sex can be determined as early as 14 weeks.
Mid-Trimester Ultrasound (18 to 20 Weeks)
Perform a comprehensive anatomical survey covering about 35 elements including the organs, face, limbs, extremities, genitals, spine, and fetal support systems (amniotic fluid, umbilical cord, cervical length, placenta).
After the ultrasound technician has captured all the data, your OBGYN will check the images for abnormalities such as congenital heart defects or cleft palate. If there are any issues with the length of the cervix or other fetal support systems revealed here, you may need to return periodically for additional ultrasounds. But for some women, this is the last ultrasound, and may even be the only ultrasound they have.
This ultrasound can take 45 minutes or longer. You may be asked to arrive with a full bladder as it puts the uterus in a more favorable position to be scanned.
Third Trimester Ultrasound (24 to 40 Weeks)
Monitor fetal growth, position, and fetal support systems (blood flow, oxygen), and evaluate the status of any issues previously identified.
This and any additional ultrasounds are at the discretion of your health care provider based on your risk factors, their standard of care, and the state of your pregnancy.
Types of Pregnancy Ultrasounds
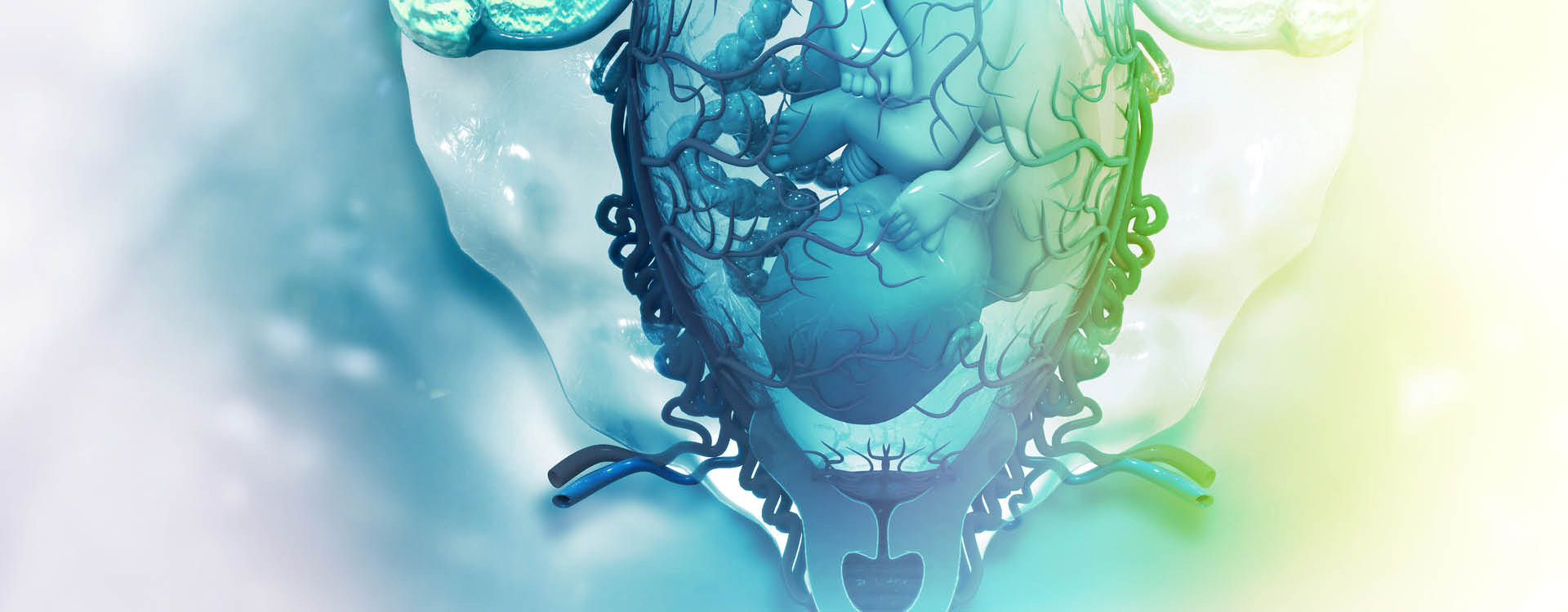
There are five types of ultrasound imaging: 2D, 3D, 4D, Doppler, and fetal echocardiography.
2D Ultrasound
2D ultrasound images are the iconic black-and-white images you may be most accustomed to seeing, and while they make look a little grainy to the untrained eye, they are considered the gold standard of diagnostic imaging. 2D ultrasound is helpful in diagnosing heart defects, issues with the kidneys, and other internal issues [*].
3D Ultrasound
3D ultrasound images add width, height, and depth to the imaging. 3D may be indicated to give a more accurate view of suspected problems, like a spinal deformity or cleft palate. The procedure is the same as with 2D ultrasound except it uses a special probe and software to create the 3D image, and a technician trained to use it, so it may not be as widely available.
4D Ultrasound
4D ultrasound, also known as dynamic 3D ultrasound, is similar to 3D ultrasound except that the images are continuously updated to create a quasi-video of the fetus.
While it may be fun to see your baby in 3D or 4D, both the FDA and American College of Obstetricians and Gynecologists (ACOG) urge parents to avoid getting 3D or 4D ultrasounds for bonding or other non-clinical reasons, and to only get them from credentialed technicians [*].
Doppler Ultrasound
Typically used in the last trimester, this ultrasound evaluates the baby’s blood flow using a transducer to listen to the heartbeat and measures the blood flow in the umbilical cord and the baby’s blood vessels. It’s indicated if the mother has Rh disease or if the baby isn't growing normally.
Fetal Echocardiography
Echocardiography is a form of advanced ultrasound that evaluates the fetus’s heart — its size, shape, structure, and how it is functioning. If your doctor suspects your baby may have a congenital heart defect they will recommend this test, which is performed similarly to a traditional 2D ultrasound.
How Ultrasounds Are Performed
Most prenatal ultrasounds (regardless of the image type rendered) are performed topically, on the surface of the abdomen, also known as transabdominal ultrasonography.
In a transabdominal ultrasound, the mother’s abdomen is coated with a harmless gel that helps the transducer move easily over the abdomen and aids with conduction. This method provides a wide view of the fetus and the pelvic organs.
In a transvaginal ultrasound, the transducer is a wand of about 2cm that is sheathed and coated with a lubricant and inserted into the mother’s vaginal canal. It’s used when your doctor needs greater detail in a smaller area. It renders a clearer view of the uterus or ovaries if a problem is suspected and is best for diagnosing conditions like ectopic pregnancy. Early ultrasounds (6-8 weeks) are often transvaginal because the fetus is only 2cm.
How to Prepare for Pregnancy Ultrasounds
Typically, a full bladder is required to get the required images in the anatomical scan. Later ultrasounds may not require a full bladder. It’s best to check with your doctor to determine how they want you to prepare.
From an emotional standpoint, it’s hard to imagine what it will feel like to see your baby for the first time.
Final Thoughts
Prenatal ultrasonography is considered safe and effective at diagnosing a wide range of fetal abnormalities and 2D ultrasound has been the gold standard in pregnancy management since the 1970s. Since then, advancements like real-time imaging and 3D ultrasound continue to enhance ultrasound’s imaging capabilities.
Whether the mother has only one ultrasound, around 20 weeks, or more depends on her health, age, risk factors, and any issues identified by her doctor.
MiracleCord believes in educating its customers so they can make thoughtful decisions that benefit their lives and those of their family now and in the future. Learn more about the MiracleCord Advantage, and request our free info kit today.
DISCLAIMER: THE INFORMATION ON THIS WEBSITE IS NOT INTENDED TO BE USED AS MEDICAL ADVICE.The materials and information contained on the MiracleCord website is provided for educational and informational purposes only, and is not intended to, and does not constitute, medical or other health advice or diagnosis, and should not be used as such. You should not use this information to diagnose or treat a health problem or disease. If you are seeking personal medical advice, you should consult with a licensed physician. Always consult with a qualified health care provider regarding a medical condition.