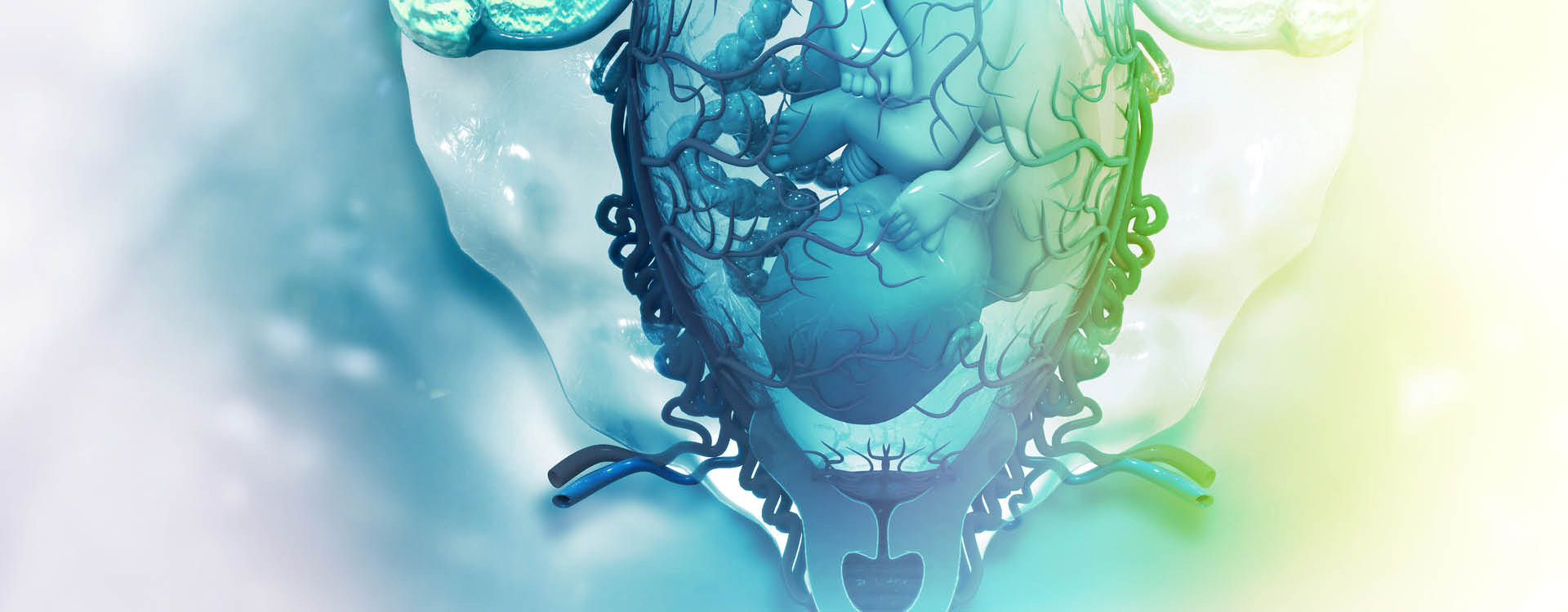
The placenta is an amazing organ that is created with each pregnancy and discarded after its job is done. It is the only transitory organ in the human body and the only one to serve two masters (mother and baby) independently. It gives the baby the blood, oxygen, and nutrients it needs to thrive, filters its waste back to the mother, and even produces the hormones that sustain the pregnancy and enable breastfeeding. When it doesn’t perform as expected, placental insufficiency is diagnosed.
What Is Placental Insufficiency?
Placental insufficiency is a condition affecting 1 in 10 pregnancies in which the placenta fails to supply enough blood, oxygen, and nutrients to the fetus. Its symptoms are hard to recognize (especially for first-time mothers) and its consequences can be life-threatening to the fetus.
Researchers don’t know exactly what causes placental insufficiency but there are a number of ways the placenta can malfunction. There may be an abnormal blood flow from the umbilical artery to the placenta; the uterine arteries may fail to remodel to support the blood flow needed to the placenta; the placenta may be too small or oddly shaped; or it may be coming away from the uterine wall.
There’s no cure for placental insufficiency; The best case scenario is to catch it early and manage it with your care team to ensure the optimal outcome for mother and baby.
Placental Insufficiency Causes
Placental insufficiency (also called placental dysfunction or uteroplacental insufficiency) can occur because the placenta hasn’t developed properly, attached to the uterine lining properly, or has become damaged, but oftentimes doctors don’t know why it has occurred [*].
What we do know is that it can be a result of certain lifestyle choices, including smoking, drinking alcohol (even 1-2 drinks a day), or using drugs like cocaine or methamphetamine during pregnancy.
The risk of placental dysfunction is also enhanced if you’ve had an untreated uterine infection, heavy bleeding, or other complication early in your pregnancy. At the tail end of your pregnancy, the risk is greater if you’re past your due date (> 40 weeks) [*][*].
Maternal medical conditions that can compromise fetal circulation enhance the risk of placental insufficiency. These include:
Placental Insufficiency Symptoms
Placental insufficiency can be very hard to detect because it often presents no symptoms. But if you’ve had a previous child, you may be more inclined to notice issues such as these that may point to an issue with your placenta:
-
Gaining less weight than expected
-
Vaginal bleeding early in your pregnancy
-
Baby moving less than expected
Talk to your care team if you’re experiencing any of these symptoms.
Placental Insufficiency Effects on Mom and Baby
Both mother and baby can experience complications arising from placental insufficiency but it is generally only life-threatening to the baby. Complications include:
-
Lack of oxygen (fetal hypoxemia) and acidosis (high levels of acid in baby’s blood) — leads to a failure to reach the baby's genetically determined growth potential, and potentially, stillbirth. Researchers believe that the physiological adaptations made by mother and baby in cases of fetal hypoxia in utero increase the risk for each of developing cardiovascular disease later in life [*].
-
IUGR (intrauterine growth restriction) — with IUGR (sometimes called FGR, for fetal growth restriction), the fetus is underdeveloped because its nutrients and oxygen have been throttled. With IUGR, the risk of spontaneous preterm labor is 3 times higher and the risk of perinatal death is 6-10 times higher than in non-restricted fetuses [*].
-
Low blood sugar (hypoglycemia), low calcium (hypocalcemia), excess red blood cells (ploycythemia), low body temperature (hypothermia) — we usually think of placental insufficiency as problems with the flow from mother to baby, but the flow from baby to mother is also compromised. Taken together, it can result in nutrient deficits and imbalances.
-
Excess bilirubin — Once the baby is born, its liver will perform the task of getting rid of excess bilirubin, but until then, it’s up to the placenta. In newborns, bilirubin above 25 mg/dl is considered dangerously high. When there’s too much unconjugated bilirubin, it can cross the blood-brain barrier and harm developing brains [*].
-
Placental abruption — a disorder in which the placenta pulls away from the uterine wall prematurely. This can cause the mother to experience life-threatening anemia, hemorrhaging, and DIC, a deadly blood clotting imbalance that occurs when clotting factors from the placenta flow too rapidly into the mother’s bloodstream. The fetus can experience distress or death. Typically, an expedient delivery is called for.
Placental Insufficiency Diagnosis
From a clinical standpoint, diagnosing placental insufficiency is a bit tricky because the terminology used to describe placental insufficiency and the techniques used to measure it are not consistent across the body of clinical and scientific research on this topic [*]. For instance, it can refer to a reduction in maternal blood supply early in pregnancy as well as a failure of the mother’s blood supply to ramp up in mid-pregnancy to meet the needs of the growing fetus.
Regular ultrasound scans are key to diagnosing and managing placental insufficiency. Doppler ultrasound can show the size and position of the placenta and fetus as well as detect blood flow between mother and baby through pathways including the umbilical artery, uterine artery, and middle cerebral artery [*][*].
MRI and advanced MRI imaging, better at revealing soft-tissue issues, may also be employed to reveal vascular abnormalities in the placenta [*].
Studies show a 38% reduction in perinatal mortality when early Doppler ultrasound is used in cases where placental insufficiency is suspected [*].
Ultrasound exams quantifying fetal growth, amniotic fluid volume, and flow and resistance to flow in maternal and fetal vessels, as well as serum biomarker assessment of growth-restricted fetuses, may predict which cases of IUGR are due to placental disease and at higher risk of stillbirth [*].
Placental Insufficiency Treatment
There is no specific treatment or cure for placental insufficiency, but there are many physiological coping mechanisms both mother and baby will perform during pregnancy to mitigate it. Early diagnosis and careful management of any underlying health conditions (like diabetes or high blood pressure) may help you carry your baby to term.
If there are signs the placenta is failing to adequately nourish the fetus, your care team will want to monitor you and your fetus closely to check on its growth and health. If you’re at term (37 weeks or more), your care provider may recommend delivery. If it’s best to deliver before term, your care team may prescribe a steroid to hasten the development of the baby's lungs, which doesn’t usually occur before week 37.
Placental Insufficiency FAQ
What is the main cause of placental insufficiency?
Placental insufficiency can’t be boiled down to one cause, and absent a maternal injury in which it is damaged, sometimes doctors don’t know why it occurs. But it most often occurs in women who have health issues that can affect blood flow, including high blood pressure, diabetes, preeclampsia, and anemia. It can also arise from inherited genetic variation or genetic mutation [*]. Women who smoke, drink alcohol, or use drugs like cocaine, heroin or methamphetamine also increase their risk of placental dysfunction.
Can a baby survive placental insufficiency?
Yes, most babies in the U.S. do go on to survive placental insufficiency, when it is diagnosed early and they are monitored by their care provider. But very early stillbirths (<28 weeks) due to placental disease may not be preventable [*].
Does placental insufficiency cause stillbirth?
Placental disease (which includes placental insufficiency and other disorders) is the leading cause of stillbirth, accounting for 23.6% of stillbirths at all gestational ages and 22.6% in late preterm and term period [*]. Placental insufficiency was responsible for 19.8% of the stillbirths in one recent study [*].
Can anything help placental insufficiency?
There isn’t a specific cure for placental insufficiency, but being aware of and managing the underlying risk factors (e.g. hypertension, diabetes, anemia, lifestyle choices, and high BMI) may help you get as close to term as possible, or prevent it entirely.
Can stress cause placental insufficiency?
Yes, stress can affect critical aspects of placental function and structures, especially early in pregnancy, and this can have a lasting effect on your pregnancy [*]. Both human and animal studies have shown timing-dependent and sex-specific effects of maternal stress on the size of the placenta, its efficiency, and its gene expression [*]. A 2016 study found that babies exposed in utero to maternal stressors like anxiety, depression, bereavement, and disasters are more likely to present with neurodevelopmental disorders and subclinical psychosocial problems [*].
Does placental insufficiency cause brain damage?
Yes. If placental insufficiency results in the fetus being underweight, undersized, or underdeveloped, the risk of cognitive, developmental, and medical complications increases exponentially [*]. This can include autism and cerebral palsy.
Can placental insufficiency be seen on ultrasound?
Ultrasound can show if your baby is growing as expected, leading your doctor to take a closer look at the placenta. Doppler ultrasound can measure blood flow through critical pathways affected by the placenta. MRI can reveal vascular abnormalities in the placenta as well.
Does placental insufficiency cause miscarriage?
It’s possible, but plenty of women diagnosed with placental insufficiency deliver healthy babies. Most miscarriages in the first three months of pregnancy are caused by chromosomal issues that preclude normal development of the fetus. That said, when the placenta doesn’t grow large enough to sustain the fetus or can’t transfer needed nutrients, oxygen and hormones to sustain the pregnancy, miscarriage can occur. This sometimes happens in cases where the placenta must support twins [*].
What are the markers for placental insufficiency?
For women pregnant with their first child, symptoms of placental insufficiency may be impossible to detect. Women who have had previous normal pregnancies may be more inclined to notice if they are not gaining as much weight or their fetus is not moving as often. In either case, regular ultrasound scans to monitor the health of your pregnancy can help your care team catch placental insufficiency early and manage it to carry your fetus as close to term as possible.
How can placental insufficiency be prevented?
If placental insufficiency occurs due to genetic anomaly, it cannot be prevented. The best thing you can do to prevent placental dysfunction is to manage any underlying risk factors. If you have a health condition that makes placental insufficiency more likely, for instance, diabetes, hypertension, preeclampsia, or obesity, talk to your OBGYN before getting pregnant, if possible. Avoid taking drugs (including those used to treat blood disorders) and drinking alcohol.
Is placental insufficiency an emergency?
Placental insufficiency can be an emergency if the fetus is not getting what it needs to survive. The earlier in pregnancy you have placental insufficiency, the more severe the downstream effects can be. In cases where placental insufficiency goes undetected, there is a major risk of preterm birth and IUGR, which are both major causes of stillbirth.
Be Prepared for the Unexpected
While every pregnant mother hopes for the best, it’s always a good idea to prepare for the unexpected. MiracleCord offers parents the ability to save cord blood and tissue from the baby’s umbilical cord in the event they or a family member need a stem cell treatment down the road.
There are more than 80 FDA-approved cord blood stem cell treatments for blood disorders, genetic diseases, immune disorders, metabolic disorders, and certain cancers, and hundreds more in clinical trials.
MiracleCord pairs the industry’s most affordable pricing with advanced processing and storage techniques to maximize your stem cell yield and protect your family.
Call 888.743.2673 to speak to a knowledgeable customer service representative now or download our Free Info Kit to learn more.
Final Thoughts
Placental insufficiency is a serious issue affecting 1 in 10 pregnancies. The earlier placental insufficiency arises, the more impact it will have on your pregnancy. But with early diagnosis and thoughtful management, you can still deliver a healthy baby. The best outcomes are seen when placental insufficiency is diagnosed between 12- and 20-weeks gestation.
DISCLAIMER: THE INFORMATION ON THIS WEBSITE IS NOT INTENDED TO BE USED AS MEDICAL ADVICE.The materials and information contained on the MiracleCord website is provided for educational and informational purposes only, and is not intended to, and does not constitute, medical or other health advice or diagnosis, and should not be used as such. You should not use this information to diagnose or treat a health problem or disease. If you are seeking personal medical advice, you should consult with a licensed physician. Always consult with a qualified health care provider regarding a medical condition.