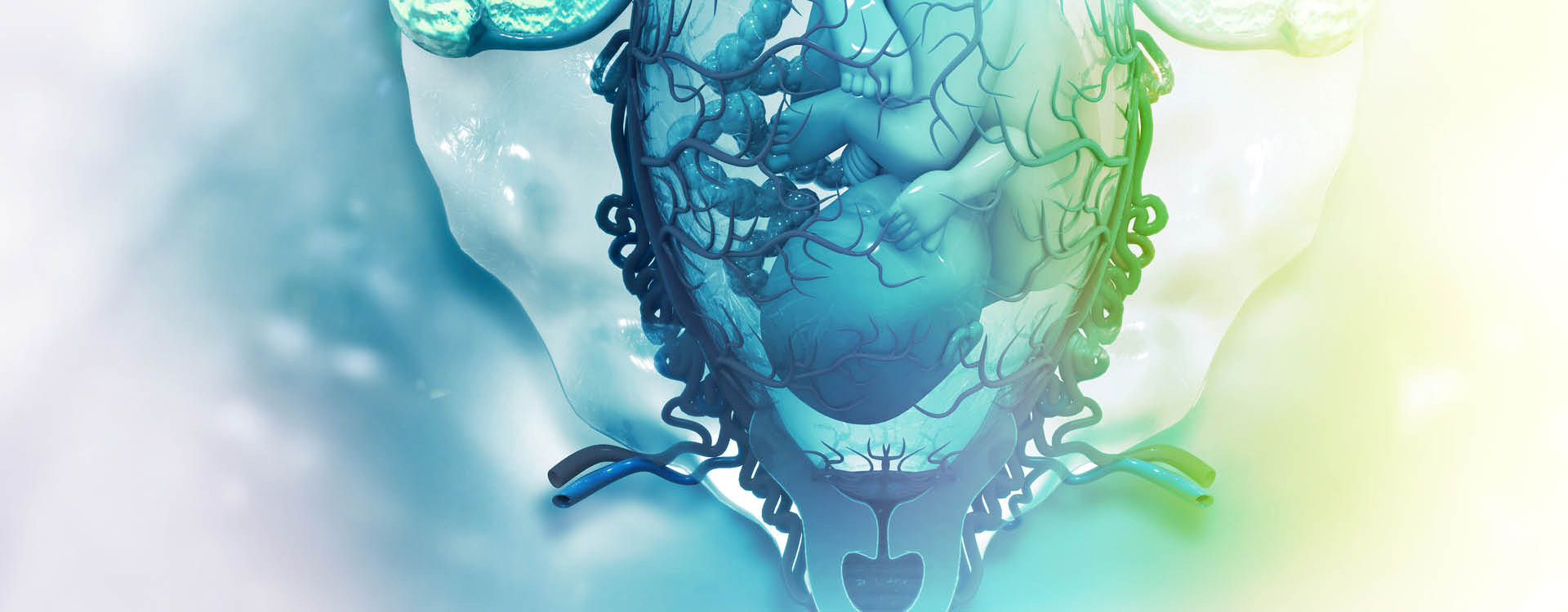
Many women experience numbness, tingling, and sometimes pain during pregnancy when certain nerves or blood vessels become compressed with the expanding womb and added weight on their joints.
But in some instances, these symptoms can also be a sign of a deficiency or issue that requires medical intervention. Here’s what to know:
Is Numbness During Pregnancy Normal?
Yes, numbness and tingling during pregnancy are very common, especially in the second and third trimesters. Some women experience it only in their hands and fingers, while others may find it radiating down their legs, on their outer thighs, or even the soles of their feet [*].
The numbness, tingling, or pain is usually caused by a combination of weight gain, fluid retention, and hormones like relaxin, which loosen ligaments to help a woman’s body expand to accommodate the growing fetus but can also lead to hypermobility. With the shifting center of balance and the added weight to support, there can be pinching or pressure on certain nerves.
The medical community refers to these issues as peripheral neuropathies. Here are the most common numbness problems pregnant women experience, by location, from head to toe.
Face Numbness During Pregnancy
If you feel a weakness or inability to move one side of your face, you may have Bell’s Palsy, a rare condition that can occur with pregnancy.
Causes
While Bell’s Palsy is rare (about 45 cases per 100,000 pregnant women), the incidence is about three times higher among pregnant women than those in the general population, with most cases occurring in the third trimester or early post-partum. Pregnant women with Bell’s Palsy also have much higher rates of hypertensive disorders such as preeclampsia, leading some to hypothesize that the build-up of fluids, edema, and restriction in the vascular structures are also to blame for compression of the facial nerve, known as cranial nerve VII [*].
The cause of Bell’s Palsy is not well understood [*]. It should also be said that not all cases of facial numbness, tingling, or paralysis are diagnosed as Bell’s Palsy [*].
Other factors researchers point to for the higher incidence of Bell’s Palsy in pregnant women are elevated clotting factors in the blood, increased estrogen and progesterone, and the weakening of the immune system in the third trimester that could lead to reactivation of a virus such as HSV or Lyme [*].
Symptoms
The upper or lower face can experience weakness or paralysis, and taste and hearing can be affected on that side as well. Numbness, tingling, and pain in the face or behind the ear are also seen, as well as trouble blinking and a dry eye on the affected side. Some women get Bell’s Palsy after childbirth, with symptoms emerging 7-10 days after the delivery [*].
Treatment
A combination of steroids, topical eye care, and antiviral medications may be administered. Treatment that begins three days after the onset of symptoms is usually associated with a full recovery, but overall, Bell’s Palsy has worse long-term outcomes in pregnant women compared with the general population [*].
Hands and Arms Numbness During Pregnancy
If your hands are feeling clumsy, and weak, or you feel numbness, tingling, or pain in your hands during pregnancy, you’re not alone. After lower back pain, this is one of the most common issues among pregnant women [*].
Causes
Carpal Tunnel Syndrome (CTS) is usually to blame for symptoms in the hands, fingers, and even the arms if the pain radiates upward. CTS occurs when there is pressure on the median nerve and reduced space in the carpal tunnel. This can happen as a result of pregnancy-related fluid retention and it is, therefore, most commonly seen in the second and third trimester [*].
The incidence of CTS among pregnant women is two to three times higher than in non-pregnant women, but statistics vary widely — from .23% to 62% of women will experience CTS during pregnancy. Pregnancy-related CTS is usually less severe than CTS in non-pregnant women and it is more likely to be bilateral [*].
Symptoms
CTS may start as numbness and become more painful, even radiating up the arm. Your hands may feel weak and the lack of sensation may make you clumsy. Some women may find their symptoms are more severe at night while others may find a certain activity makes it worse.
Treatment
Because CTS tends to be less severe in pregnant women than their non-pregnant counterparts, treatment is usually conservative. Your care team may tell you to avoid repetitive maneuvers or wear wrist splints to maintain a neutral position of the wrist. In some cases with more severe symptoms or functional impairment, your doctor may prescribe analgesics, a low-salt diet, or a local steroid or lidocaine injection [*].
One of the big questions about pregnancy-related CTS is when and if it resolves after the baby is delivered. Most often, it does resolve after the birth but not right away. Studies show that the later the symptoms appear in pregnancy, the more likely they are to resolve in a few months after delivery [*].
One study found that women who got CTS earlier in pregnancy and had greater weight gain during pregnancy were more likely to have persistent symptoms of CTS after pregnancy [*]. About half the women with pregnancy-related CTS in another study still had symptoms three years after delivery [*].
Lower Body Numbness During Pregnancy
Numbness, tingling, or pain in the legs, lower back, buttocks, or feet during pregnancy is also common among pregnant women.
Causes
The most common neuropathies in the lower body are sciatica, meralgia paresthetica, and tarsal tunnel syndrome (TTS). Nerve compression is the root cause of all of these problems.
Sciatica
Sciatica may be caused by the loosening of your ligaments from the hormone relaxin and changes in your center of gravity as the fetus grows. Sometimes the position the baby is in can exert enough pressure to cause sciatica [*].
Meralgia Paresthetica
Meralgia paresthetica, also known as Bernhardt-Roth syndrome, occurs when the lateral femoral cutaneous nerve (LFCN) gets compressed or pinched. The LFCN begins in the lower spine and travels under a pelvic ligament down the leg. A pregnant woman’s growing belly and increased weight can put pressure on the groin to cause meralgia paresthetica.
Women who are overweight or obese are at increased risk, and women with diabetes are seven times more likely to develop it [*]. If you have a scar from a prior abdominal surgery or c-section, that can also increase the risk [*].
Tarsal Tunnel Syndrome (TTS)
TTS is the evil twin of CTS. It’s caused by inflammation of the posterior tibial nerve which runs along the inside of the ankle and foot [*]. Ligaments in the feet may relax with pregnancy, and with the added weight to support and shift the center of balance, the arch of the foot can drop and cause inflammation of the posterior tibial nerve.
Symptoms
While the symptoms of these lower body numbness issues are certainly not pleasant, there’s no risk to the baby if you have any of these conditions. These symptoms are the first clue you might have sciatica, meralgia paresthetica, or TTS.
Sciatica
Sciatic pain can range from mild numbness or tingling to a burning sensation or excruciating jolt of pain that radiates down the back of your thigh. It occurs when your spine compresses in a way that pinches the sciatic nerve — the largest nerve in the body and the main conduit to the legs.
Meralgia Paresthetica
The skin of the outer thigh will feel very sensitive to light touch and you may experience numbness, tingling, or pain there. The movement of the leg will not be impacted as the affected nerve is only sensory. Without intervention, symptoms may worsen as the pregnancy progresses [*].
Tarsal Tunnel Syndrome
Tingling or burning sensations or numbness on the sole of your foot, weakness, or a sharp pain that radiates to the arch and sole of your foot are common symptoms of TTS. Risk factors for TTS include diabetes, hypothyroidism, flat feet, and hyperlipidemia (high levels of fats in the blood) [*].
Treatment
Here are some specific things you can do to mitigate lower body numbness issues, along with general recommendations to avoid such issues:
Sciatica
- Sleep on your side opposite the pain with a pillow between your knees.
- Avoid standing for long periods.
- Use a warm compress, or take a warm shower, alternating with a cold pack if it feels good.
- Avoid lifting heavy objects.
- Swim — or even just float — to enhance blood flow and take the pressure off the sciatic nerve [*].
Meralgia Paresthetica
- Wear loose clothing.
- Avoid running, walking, or biking for long periods.
- Do stretching and strengthening exercises to relieve the pressure, like clamshells and lunges.
- Physical therapy such as myofascial release, dry needling, and joint mobilization.
- If pain persists and is not resolved with PT, your doctor may recommend a steroid injection or medication such as Gabapentin, or isolated nerve cryotherapy [*].
Tarsal Tunnel Syndrome
- Rest.
- Ice.
- Physical therapy.
- Massage.
- Exercises such as heel-to-toe raises, calf stretches, and balancing exercises, as recommended by your trainer or doctor [*][*].
Ways to Prevent Numbness in Pregnancy
There are a number of general things you can do to treat — or perhaps avoid altogether — these potentially debilitating issues.
- First and perhaps foremost, stay active during your pregnancy. Gentle yoga, swimming, working with a trainer who specializes in pregnancy fitness, or even walking briskly every day will go a long way to bolstering your circulation, helping your body cope with the added weight, reducing the potential for complications, and helping you recover your fitness and well-being faster after delivery [*].
- Avoid foods that can cause fluid retention and drink plenty of water.
- Eat a balanced diet and take vitamin supplements as recommended by your care team.
- Consider working with a physical therapist, massage therapist, or Chiropractor to help you cope with your postural changes and balance during your pregnancy [*].
When Should I Be Worried About Numbness During Pregnancy?
In most cases, feelings of numbness or tingling can be attributed to compressed nerves in the course of pregnancy, but there are a few serious conditions associated with numbness and tingling during pregnancy that can compromise the health of both you and your baby. Your doctor may order blood tests to rule out disorders affecting nerve function:
Iron Deficiency Anemia
This can lead to restless leg syndrome and a tingling or crawling sensation in the legs [*].
Vitamin B12 or Folate Deficiency
If you have numbness or tingling along with extreme fatigue, disturbed vision, mouth ulcers or sore tongue, brain fog, or loss of appetite, contact your doctor [*].
Preeclampsia
The swelling caused by preeclampsia can cause numbness. If you also have headaches, vision changes, abdominal pain, nausea, or vomiting, contact your care team immediately.
Gestational Diabetes
You may experience numbness, tingling, or pain in your hands and feet. If you also have the need to urinate frequently, are very thirsty, hungry, or fatigued, contact your care team immediately [*].
Blood Clot
Numbness or weakness on one side of your body can be a sign of a blood clot. A deep vein thrombosis (DVT) is rare during pregnancy but may also present with pain in the calf or inner thigh or swelling of an arm or leg [*].
If you experience a rapid onset of symptoms or have numbness or tingling in tandem with other unusual symptoms such as these, contact your care team right away.
Keeping Families Safe
MiracleCord makes it easy and affordable to save your baby’s precious cord blood stem cells. Our customers tell us they appreciate the added layer of insurance against a future disease treated by stem cell transplant.
MiracleCord was recognized by Global Health and Pharma as the Best U.S. Cord Blood Bank for its technology, pricing, and service. Learn more by downloading our Free Info Kit or calling 888.743.2673.
The Bottom Line
Numbness and tingling are common in pregnancy and usually resolve after delivery, but it can take some time.
It’s also seen in some cases in the weeks after delivery, sometimes as a result of the delivery but not always.
In either case, it’s best to discuss these symptoms with your doctor promptly to mitigate the potential for nerve damage and ensure they’re not related to a more serious complication of pregnancy.
DISCLAIMER: THE INFORMATION ON THIS WEBSITE IS NOT INTENDED TO BE USED AS MEDICAL ADVICE.The materials and information contained on the MiracleCord website is provided for educational and informational purposes only, and is not intended to, and does not constitute, medical or other health advice or diagnosis, and should not be used as such. You should not use this information to diagnose or treat a health problem or disease. If you are seeking personal medical advice, you should consult with a licensed physician. Always consult with a qualified health care provider regarding a medical condition.